The Birth of Audrey: Mariah’s Story
nataliebroders.com > blog >
Natalie Broders
August 5, 2019
Written by:
Birth is unpredictable.
I spent two days off-and-on with Mariah and Seth. She was dilated to 7cm, but contractions had stopped. I went to her at the birth center, stayed the night, then returned home to give her some space to get back into her groove — while her wonderful midwives worked their magic.
A little after midnight, I got the call to come back. I jumped out of bed and raced to the hospital (they ultimately transferred from the birth center).
She was pushing AS I WALKED IN. I panicked, threw my backpack down, and grabbed my camera. Spoiler alert, I made it!
Her early labor was very long (days!) and slow, but extremely fast at the end.
You can read Mariah’s birth story in their own words below.
PS: have you ever seen so much vernix?! OMG
Mariah’s Birth Story
41 years old, married, mother to one 6 year-old daughter, Victoria.
This is my second (and last) baby, although sixth pregnancy (3 ectopics, one missed miscarriage).
Baby Audrey Rosalind
7 lbs, 13 oz. 20 inches.
Alma Midwifery Birth Center in Portland, OR
and Providence Portland.
Labor
We started trying natural induction methods at my birth center when I hit 41 weeks. I had been “ready to go” for at least two weeks – at my 39 week appointment I was 3cm dilated, 50% effaced, and she was at a -1 station. I went into labor with my first daughter at 39 weeks, so I thought Audrey would be early too.
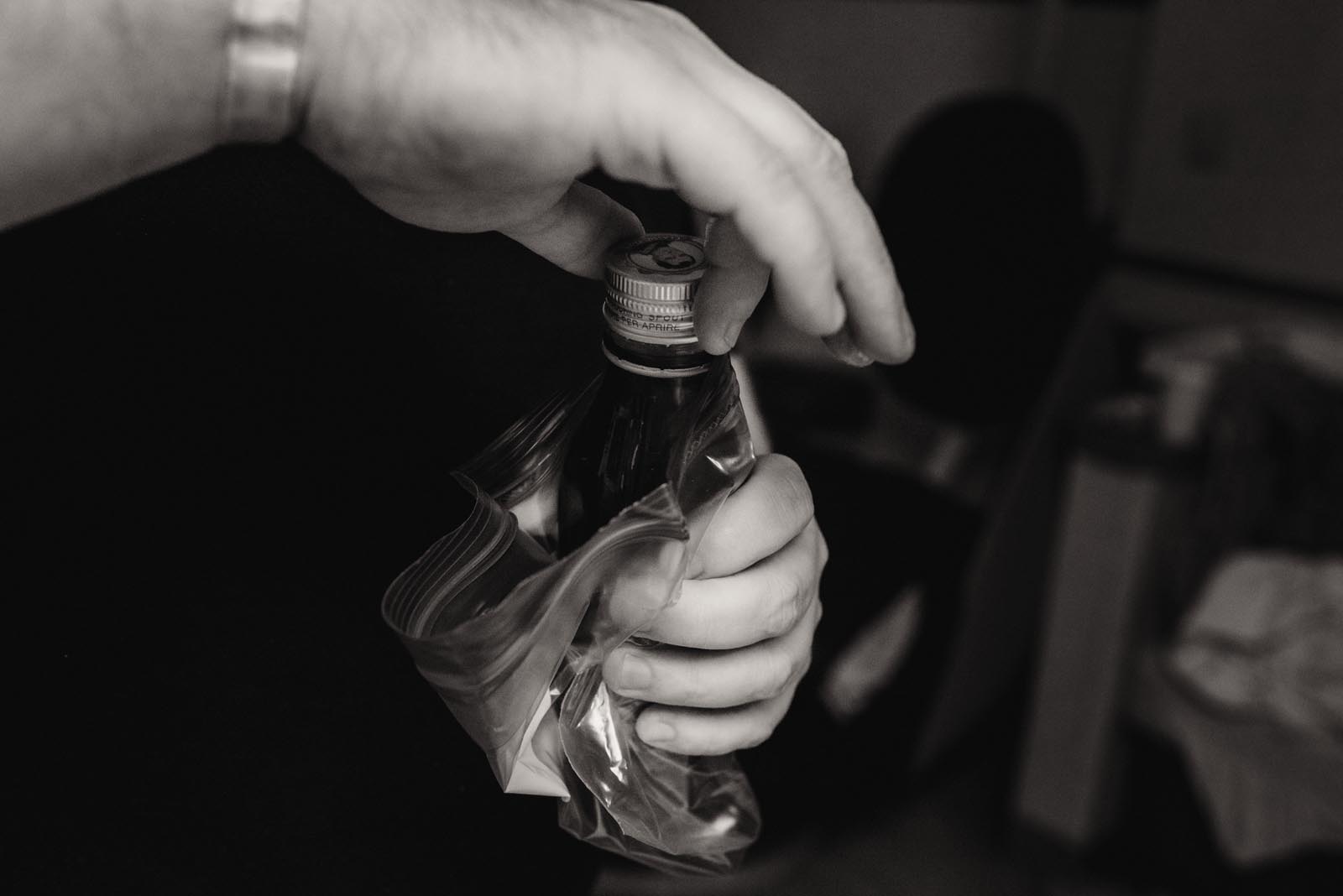
But by 41 weeks nothing was happening. I first tried induction by drinking cotton root bark, walking and breast pumping. The next morning, the midwifes broke my water at the birth center. I did more cotton root bark and breast pumping throughout the day, but active labor still wouldn’t kick in, and I wasn’t feeling contractions even though I was between 6 – 7 cm dilated.
The next day we tried some more methods, including an enema and acupuncture, but by the end of the day I was exhausted and still hadn’t progressed.
We transferred to the hospital where they started me on a low dose of Pitocin. It took about an hour and a half to kick in (thankfully I got a nap), and once the contractions kicked in they were incredibly intense and close together.
With my first baby, I had back labor and delivered unmedicated. It was pretty long and awful, and I was really looking forward to not having back labor this time.
The pitocin changed everything. When the contractions started, I was able to keep on top of them by focusing on my breathing, counting seconds of my breath, in and out. The contractions were lasting for a minute and were a minute apart.
As they got more intense I sat on a yoga ball and bounced. I remembered Ina May recommending “horse lips” so that’s what I did to get through contractions for that period. Then they ramped up and I wanted to get in the bathtub to see if the water would ease them. But when I got into the bathroom the pain of contractions and the warmth of the bathroom combined to trigger my vasovagal fainting reaction. I got lightheaded and started to lose consciousness and had to lie on the floor. My support team got me back into the main room and on the bed, where I continued laboring on my hands and knees.
The contractions became too strong for “horse lips” and I started groaning and moaning through them. I remembered hearing (Ina May again?) that low tones were more effective than high screechy ones, so I tried to keep my pitch low.
The pitocin contractions were just awful, awful, awful. There was no way out but through, but that thought was frightening. It was scary as they ramped up, not knowing how bad they could actually get. Each contraction was like cramping, burning, and pain, encompassing my whole consciousness.
They were so unbearable and it felt terrifying to me that there was no way to say, “Stop! No thanks! I’m done!” I slightly regretted not asking for an epidural because it was so freaking awful, but I also suspected that I was in transition – because it was so freaking awful. Sure enough, they checked and I was almost ready to push. This all apparently took place within the span of about 45 minutes.
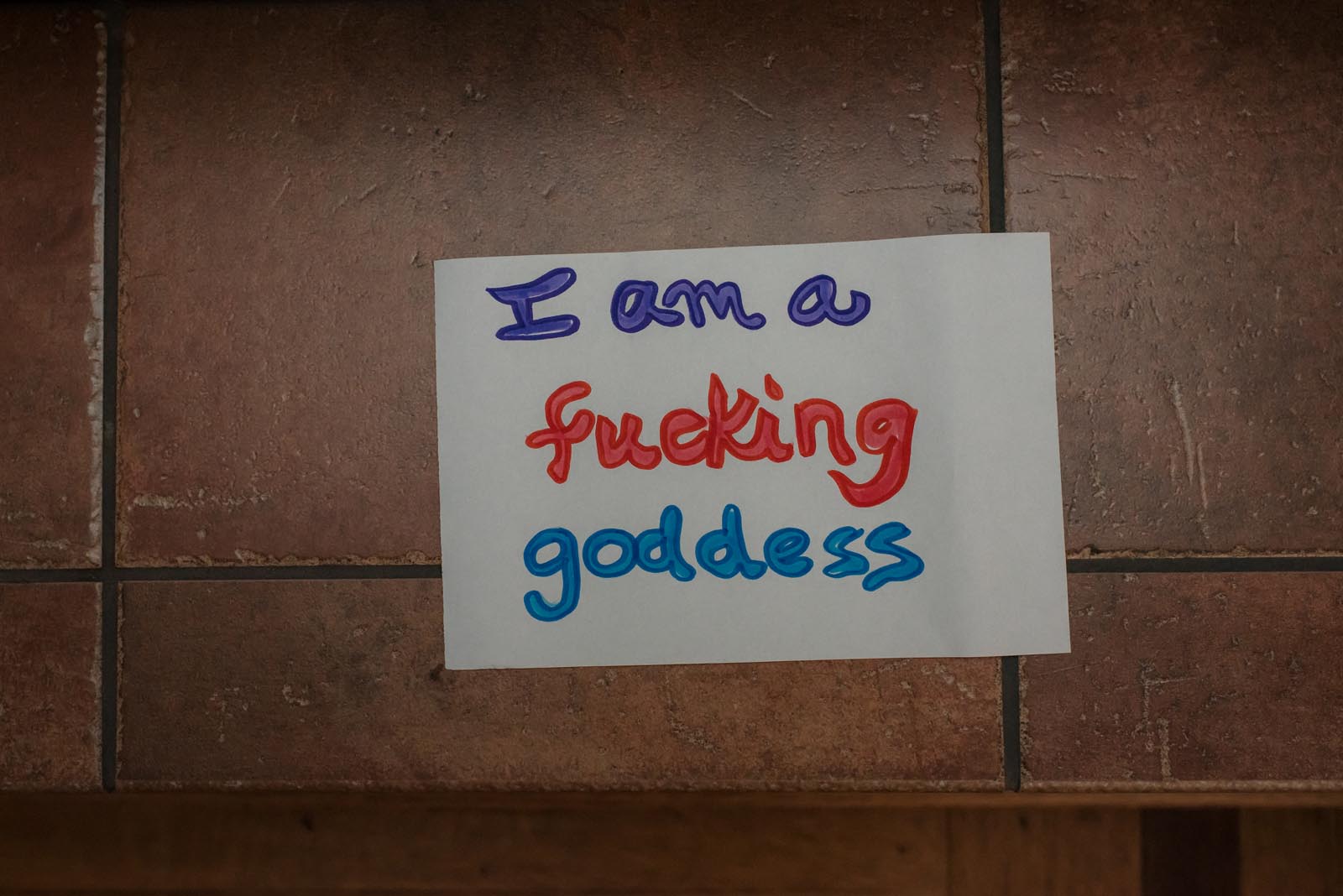
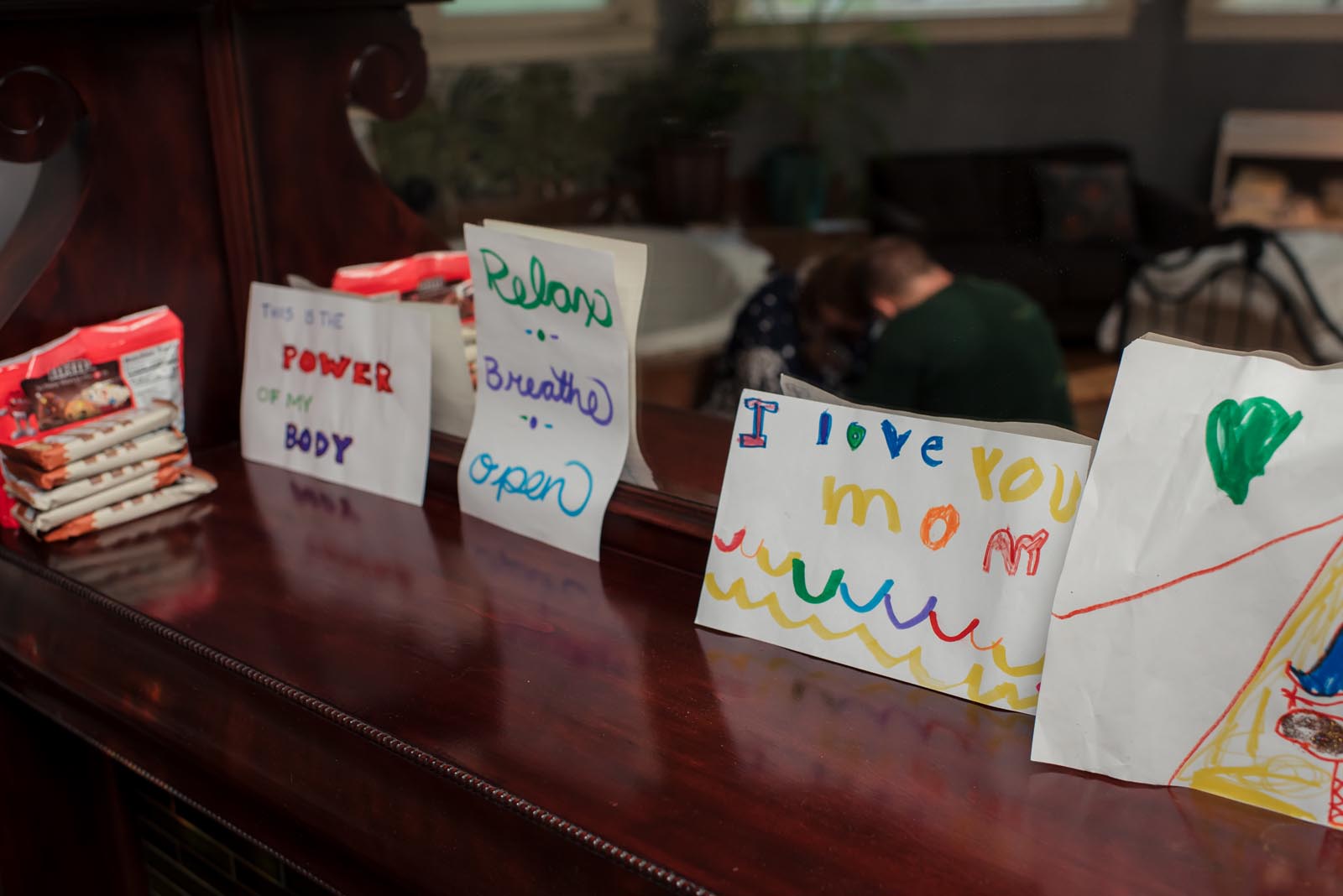
My husband Seth was a great source of support. He helped by saying some of my mantras back to me, and most importantly, allowed me to grip his hands as tightly as humanly possible through the worst of the contractions. I also had a great nurse, a hospital-provided doula, and both the hospital midwife and my midwife from Alma for the delivery.
Preparation
I had been listening to a lot of birth stories on The Birth Hour podcast leading up to labor, so I tried to remember tactics for getting through contractions that other mothers said had helped them. I read some chapters from Birthing From Within. I prepared a lot less for this birth than my first.
Birth
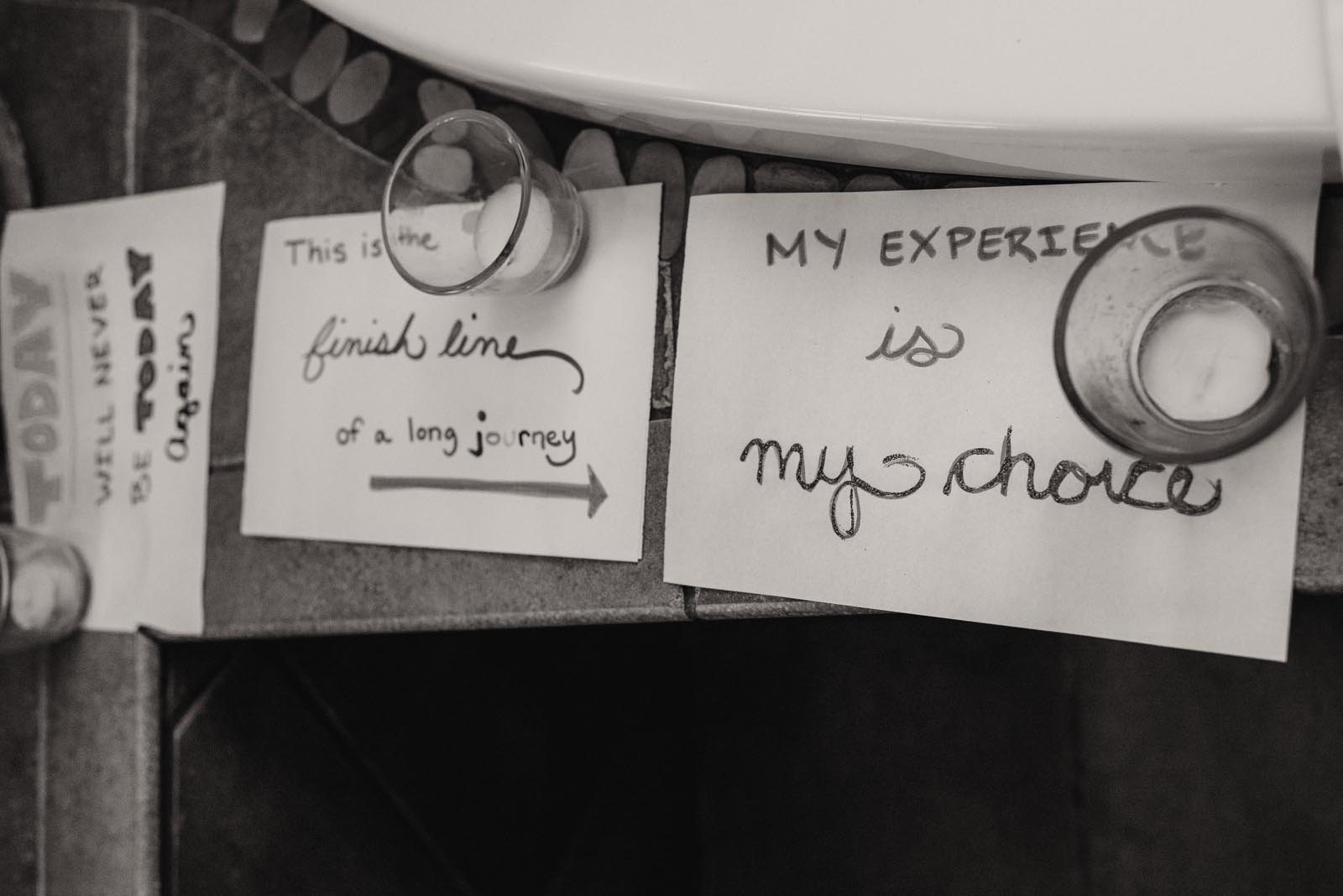
It was fast. Intense. I moved from being on all fours on the hospital bed to sitting in the birthing chair, but it didn’t feel quite right to me. After a while I got back down on my hands and knees on the floor. Even though it was uncomfortable on my arms/legs it just felt like a better position.
According to the hospital, I had approximately 45 minutes of active labor – it may have been slightly longer. The timeline I put together is:
9:00 pm: arrive at hospital
9:45 pm: all hooked up to IV and monitors
10:00 pm: nap
11:30 pm: awoken by contractions kicking in
12:40 pm: Natalie and Laura (Alma midwife) called… I think this coincided with being checked and being almost fully dilated
1:37 am: Audrey is born
I remembered a birth story where someone said that a lot of women “like” the pushing part because it feels productive. Once I got that into my mind, I told myself with each push that I liked it! That the baby was coming out! With each push, my moans turned into growling grunts. It was very animal.
With my first, I never had the urge to push. This time I almost had to hold myself back. I tried to push a couple of times in between contractions and there was a huge difference in productivity. Mentally, part of me wanted to push as hard as possible with each contraction and get her the hell out, and part of me wanted to try going slower to avoid any damage to my body. Near the end, the hard pushing won out.
One funny thing was that everyone (radiologists, midwives) estimated that Audrey would be close to 9 lbs. As I was pushing, I kept thinking, “this is a big baby. This is what it’s like to push out a 9 pound baby.” She ended up being only 3 ounces heavier than my first was.
When she was born, I think I said, “hello baby! Hello Audrey!” I felt so happy to finally have her in my arms and to see what she looked like. I was so relieved that she made it through the 41+ weeks and was healthy and here.
I felt amazing. With the contractions over and the baby out it was like the previous two hours had never happened. I felt so proud of myself for getting through those nightmare pitocin contractions. I was glad that I didn’t have an epidural because I could immediately move and feel normal. Audrey was amazing – bright eyed, looking around, very aware. She looked just like baby Victoria.
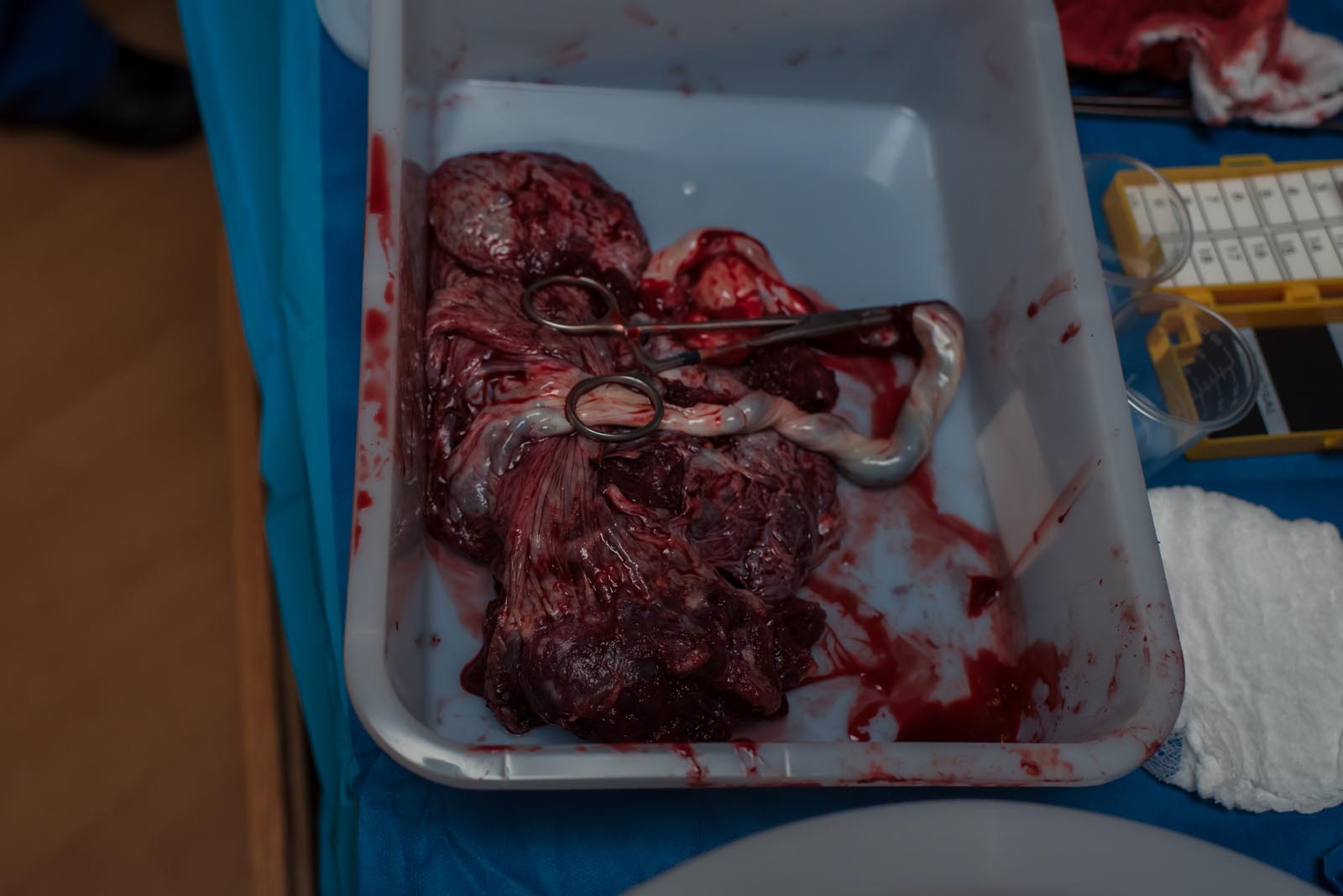
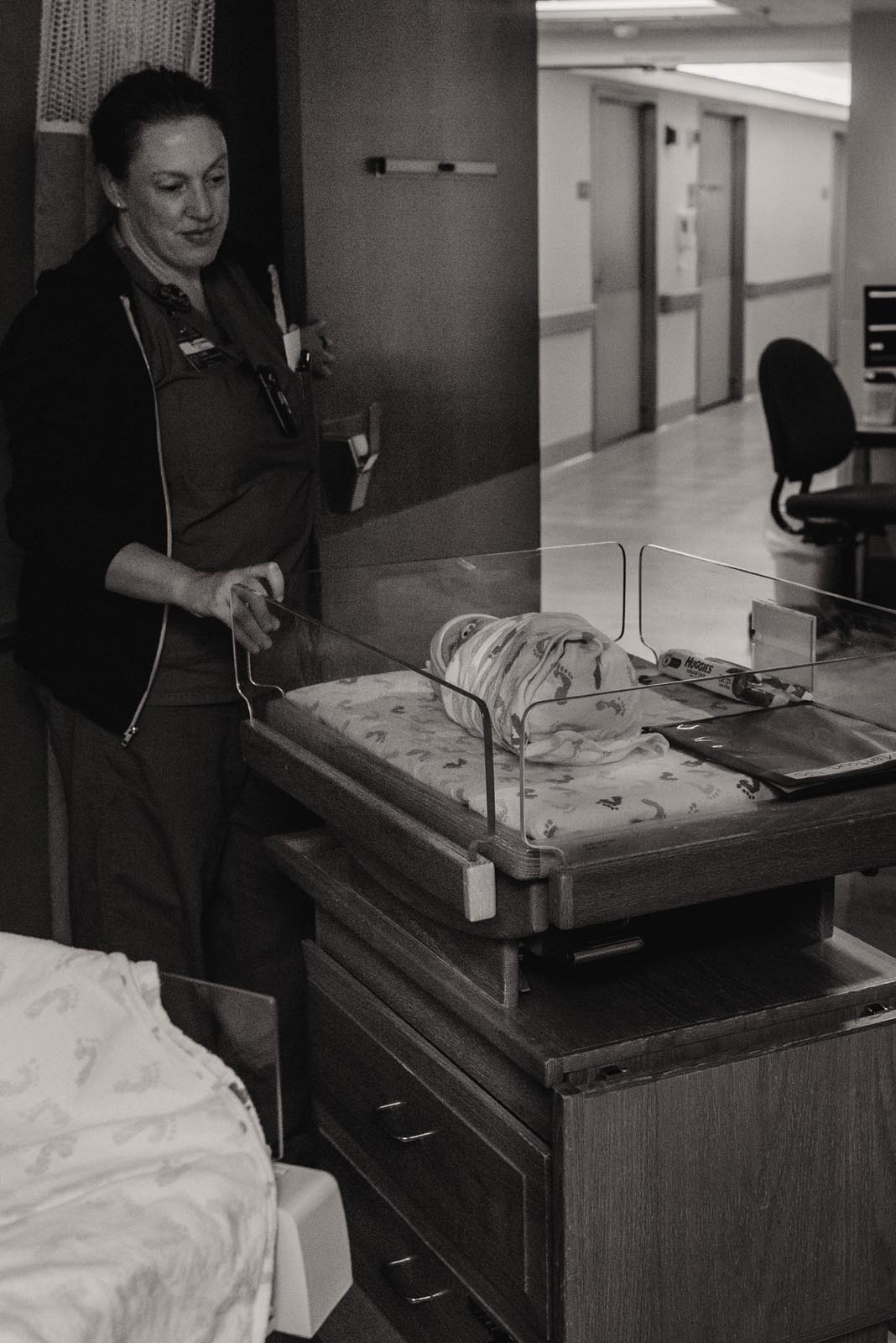
The immediate relief once Audrey was out of me and in my arms was the best part. It’s also nice to be wheeled into a recovery room after surgery. I’m glad that we were at the hospital after all so the placenta could immediately be taken care of.
People were amazed by her alert eyes looking at everything. I remember Seth cutting the cord. But there was a lot of activity going on because of my retained placenta.
I reaffirmed to myself that I am a badass. And also I don’t think acupuncture works for me.
Retained Placenta
After Audrey was born my placenta wouldn’t come out. We were prepared for this to happen as my placenta was also stuck with my first and I ended up hemorrhaging 2000 ml of blood as I was transferred to a hospital and got a D&C.
This time, I began to hemorrhage after the attending midwife pulled on the umbilical cord. Eventually she had to put her hands up into my uterus to get it out manually, which was incredibly painful and had me screaming.
Then they rushed me to the OR to do a D&C and make sure everything was removed. Later, the attending OB told us that my uterus is like an orange that won’t peel, that this is going to happen every time, and that we shouldn’t have more kids. This time I lost 2500 ml, topping my old record.
The OR was lovely and everyone was very nice and focused on making sure I was okay. And quite frankly, after pushing a baby out of your vagina and then having someone’s hands up inside your uterus, it’s really pleasant to just lay back on a table and let people work on you while you’re a bit hopped up on drugs.
Expectations about birth
The pitocin contractions were no joke. They did not ramp it up quickly, but still I wish I had advocated for myself and asked them to go even slower, knowing that I was at 7 cm already and I probably just needed a little push to go into labor.
After laboring with Victoria for over 24 hours, with both back labor and my water breaking at the beginning of labor, I wanted this labor to be a chance at a “redo.” I was hoping for no back labor, that my water would break during active labor, and that I’d get maybe and awesome water birth in a big tub and a relaxing birth center stay.
Instead I got the hospital, pitocin, a little back labor, and another retained placenta, ending in another hemorrhage and trip to the OR. After my first, I thought “I could do that better.” With Audrey, I proved to myself that no, no I can’t. The peaceful birth center dream will never be a reality for me, even if we were to have more kids. I’m at peace with that.
Both of my labors could be seen as traumatic, but it doesn’t feel that way to me. In both instances I felt like I came through something very difficult, even dangerous, and I prevailed. A huge part of my positive feelings are due to my support team. One of the reasons I’ve gone through midwives and birth centers is because I feel like they are attuned to what I want in a birth and are inherently supportive, whereas I have been concerned that going the more medically-focused route would mean more advocating/arguing. That said, I was really impressed with my experience at Providence Portland.
Dad’s Perspective
When labor finally started, I felt a sense of relief. Since we had so many caring professionals around us, mostly what I felt was that I was happy that things were actually happening after we waited two days for labor to start, one week since the due date, 9 months since we figured out we were pregnant, and three years since we started trying.
You worry about worst case scenarios, and at some point you have to put yourself in the hands of fate, and I think that’s where I was at when Mariah’s labor started. I also felt that there was finally clear, unambiguous support that I could give. Because waiting is difficult.
I’m always amazed at the confidence I have in Mariah’s abilities. I thought she was extremely focused and extremely prepared to do what she needed to do. I was really only there to help her understand it was okay to be vocal, and that was probably going to help.
The high point (for me) was when labor actually started. We had a lot of people who were on call for us, and that definitely made me a bit more impatient than I normally would have been. Also seeing my daughter born was a high. But the labor starting was the end of all the waiting.
The lows are being a birth partner and constantly having to filter your thoughts and pick your words very carefully — because you’re there for support, and it’s not about you.
When I saw Audrey for the first time, I thought she was incredibly strong. She could hold her head up and her eyes were wide open. My feelings of holding her for the first time were great, also relief, but also tinged with the knowledge that there were things going on with Mariah.
Portland Birth Photographer
Birth Doula & Videographer
Natalie Broders is a birth photographer, birth videographer and birth doula located in Portland, Oregon. She lives on a farm with her husband and 2 kids. They raise chickens and love to garden. Natalie loves babywearing, cloth diapering and is passionate about her work as an advocate for birthing people as a labor and birth doula. She had one of her babies at a birth center and her second baby was born at home, in water.